Our recent publication, “Stress response pattern of heart rate variability in patients with functional somatic syndromes,” investigates the intricate dynamics of heart rate variability (HRV) during mental arithmetic stress in individuals with Functional Somatic Syndromes (FSSs).
The study unveils a distinct “flat” vagal stress response in severe FSS patients, providing critical insights into their altered physiological state compared to healthy controls. These findings not only contribute to a deeper understanding of FSS pathophysiology but also open avenues for potential diagnostic and therapeutic interventions based on stress response patterns. Read the full article here.
Saka-Kochi, Y., Kanbara, K., et al. Appl Psychophysiol Biofeedback (2023).
https://doi.org/10.1007/s10484-023-09608-z
Summary
Study Objective
- Explore HRV stress response patterns in Functional Somatic Syndromes (FSSs) during mental arithmetic stress, comparing them with healthy controls.
- Evaluate autonomic pathophysiology, focusing on reduced HRV in stress-related FSSs.
- Address the unclear understanding of autonomic stress response patterns in FSSs.
Major Findings
- Severe FSS patients display an altered “flat” vagal stress response, maintaining low HRV throughout relaxation, stress, and post-stress, contrasting with the pronounced stress response and recovery in healthy controls.
- FSS patients show elevated mood questionnaire scores, prolonged illness duration, and reduced daily functionality compared to controls.
- The study suggests the potential diagnostic and therapeutic relevance of altered stress response patterns in FSSs, shedding light on the stress-illness relationship.
Significance and Implications
- Emphasizes assessing both stress reactions and recovery processes for a comprehensive understanding of FSS patients’ physiological status.
- Contributes to developing diagnostic and therapeutic approaches for FSSs, highlighting the dynamic changes in autonomic function induced by stress.
- Offers valuable insights into the shared pathophysiological mechanisms of FSSs and their connection to stress, paving the way for further exploration of stress-related diseases.
Methods
Study Participants, Diagnostic Criteria and Classification
- Cross-sectional case-control study involving 79 patients (13-74 years) diagnosed with FSS and 39 healthy controls.
- FSS diagnoses were based on three criteria: somatic symptoms without organic or psychiatric explanation, subjective-symptom rating score >3/10 lasting >6 months, and symptoms causing difficulties in social or daily activities (GAF score < 80).
- Patients with FSS were categorized into five groups based on diagnoses, including fibromyalgia syndrome/chronic fatigue syndrome, functional gastrointestinal disorders, chronic pain, musculoskeletal disorders, and others.
Physiological Measurements and Data Processing
- Heart rate variability (HRV) parameters, mean inter-beat interval (IBI), low frequency power (HRV-LF), high frequency power (HRV-HF), were measured during three periods: baseline, mental arithmetic stress task, and post-stress recovery (5 min. each, total 15 min).
- HRV parameters were analyzed using the Kubios HRV software (KUBIOS OY), and mood assessments were conducted using the Profile of Mood States (POMS) test.
Findings
- Patients with FSS exhibited significantly lower HRV parameters (IBI, HRV-LF, HRV-HF) compared to healthy controls during baseline, stress, and post-stress periods.
- FSS group displayed a “flat” stress response with lower HRV-HF at baseline, reduced stress response, and no post-stress recovery, in contrast to healthy controls.
- The reactive stress response pattern of HRV-LF was observed in the FSS group, indicating chronic vagal dysfunction possibly linked to an exaggerated sympathetic stress response.
- The control group showed typical stress response patterns with decreased HRV during stress and subsequent recovery, while the FSS group displayed abnormal patterns as above.
- These findings provide an overview of the stress response patterns in patients with a severe spectrum of FSS.
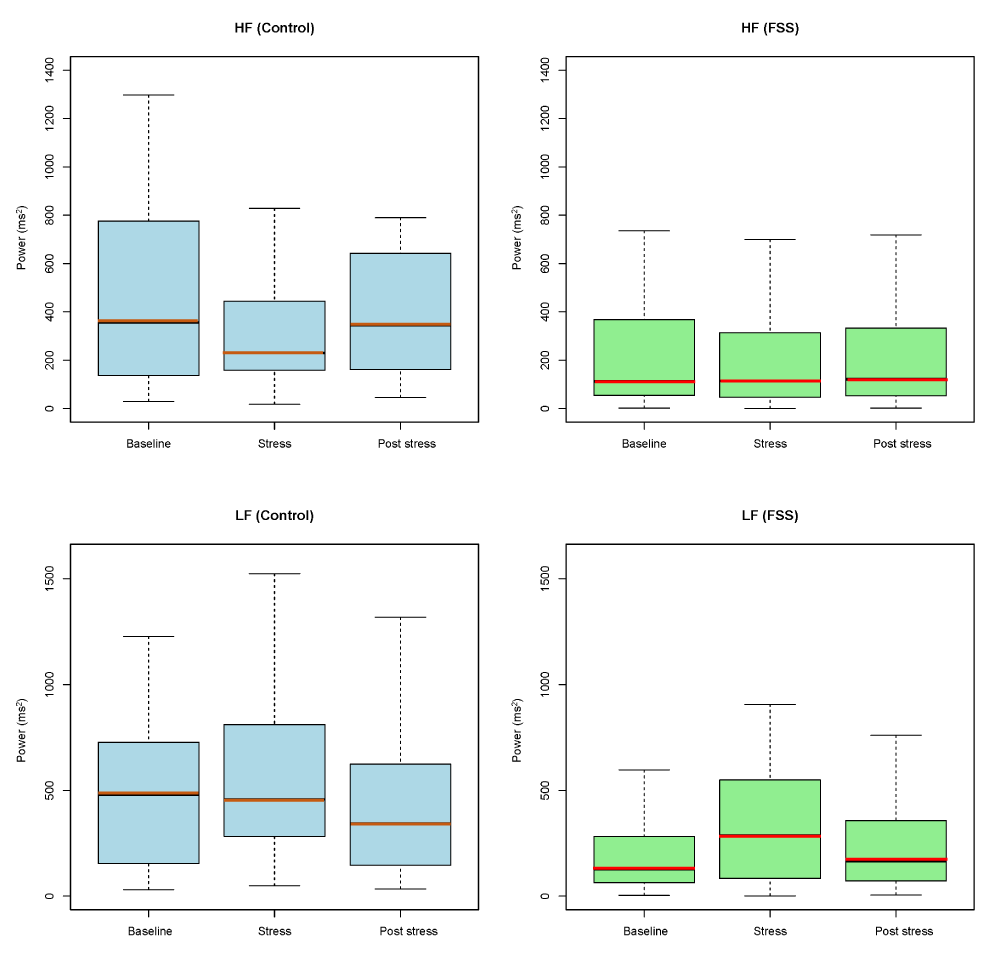
Figure illustrates changes in the LF and HF components of heart rate variability (HRV) before and after mental arithmetic stress in individuals with Functional Somatic Syndromes (FSS, n = 79) and healthy controls (n = 39).
The LF (low frequency) and HF (high frequency) box-and-whisker plots compare HRV between control and FSS groups. Each box represents the middle 50% of the data, with the line inside indicating the median. Whiskers depict the range of values within a specified limit. HRV: heart rate variability; LF: low frequency; HF: high frequency; FSS: functional somatic syndrome; Baseline: relaxation baseline.
Discussion
Stress Response Patterns of HRV in FSS
- Patients with severe FSS exhibited a unique “flat” vagal stress response pattern compared to healthy controls.
- While healthy controls demonstrated a pronounced stress response pattern with a significant decrease and subsequent recovery in HRV-HF, the FSS group displayed a diminished stress response, and no recovery was observed.
- In contrast to the flattened pattern in HRV-HF, patients with FSS displayed a reactive stress response pattern in HRV-LF, marked by a significant increase during stress and subsequent recovery, differing from the control group.
- The study suggests a chronic vagal dysfunction, possibly rooted in an exaggerated sympathetic stress response, in patients with severe FSS, representing a novel finding in stress response patterns.
Clinical Implications and Insights
- Significance of altered stress response patterns in severe FSS for diagnosis and treatment, offering potential biomarkers for assessing disease severity.
- Proposed a hypothesis that the vagal stress response pattern evolves with the duration of illness, connecting prolonged distress to lower and flatter HRV-HF.
- Limitations, suggesting the need for future multi-center studies, longitudinal interventions, and extended recovery periods to delve deeper into the complexities of HRV patterns in FSSs.
This work was supported by JSPS KAKENHI Grant Number 20K03462.
(Kanbara K, et al. 2020-2023 “Pattern analysis of physiological stress response using machine learning and construction of clinical model of stress response.”)
